This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
Mentioned here are my learning points, both theoretical and practical surrounding this patient:
-I performed a full sensory and motor system examination on this patient and recorded my findings below. Additionally, I learnt how to localize the level of spinal cord lesion based on my findings. Beaver's sign was a learning point for me as well.
-Learnt how to differentiate LMN bladder from UMN type bladder
-Learnt about NMOSD (Neuromyelitis Optica Spectrum Disorder), its symptoms and possible clinical findings
The patient came to the OPD with chief complaints of:
-Urinary retention since 1 day
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 1 year back when she developed headache, fever and acute urinary retention. Following the development of these complaints, she came to our hospital where she was evaluated and diagnosed with transverse myelitis.
The evaluation along with the blog contents of the previous admission at our college have been added here below:
(Courtesy of Vasishta: https://vasishta175.blogspot.com/2022/02/admission-3-and-6-amc-bed-1-patient.html?m=1 )
Patient was brought to casualty with c/o :-
-Headache since 10 days
-Fever since 10 days
-Acute urinary retention since 5 days
22yr old female , farmer by occupation
Patient was apparently asymptomatic 10 days back , then she developed a headache, diffuse in nature, occipital region predominantly, gradual in onset , dragging type , radiating to neck, aggravated on talking , rotating the head , relieved on medication
Associated with nausea
- Phonophobia present
- No h/o Photophobia , Lacrimation
- C/o Fever since 10 days , High grade fever associated with chills and rigors, Continuous , relieved on medication , gradual in onset
- Pt c/o Vomitings , associated with nausea , Non projectile , not associated with blood
- After 5 days Pt c/o urinary retention ( acute ) , able to feel fullness of bladder , not able to pass urine , relieved after passing foleys
-No c/o cold , cough
- 5 days back Pt attenders c/o Altered Sensorium which lasted for 5 mins . Not able to recognise persons , place, time
- Had Weakness of lower limbs for 4 days . Spontaneously resolved .
- patient was not able to walk on her own during the weakness episode
- No seizures , weakness
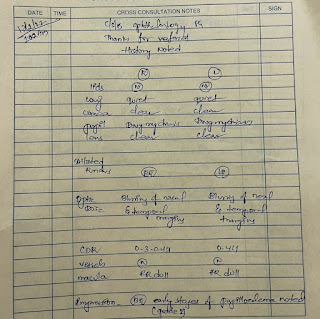
Ophthalmology referral:-
Impression:-
Early changes of Papillodema noted ( Grade 1)
Personal history:-
Married female
Appetite - decreased , improved since yesterday
Bowels- Constipation , relieved on medication
Micturition- abnormal
Addictions:- No addiction
General examination:-
Pt is c/c/c
Pallor present
No icterus , cyanosis , clubbing , odema, lymphadenopathy
Vitals:-
Temp:- Afebrile
PR:- 110bpm
RR:- 14 /min
BP:- 100/60mmhg
Spo2:- 97%
GRBS:- 133mg%
Systemic examination:-
CVS :- S1S2 heard , No murmurs
RS:- BAE present
PA:- Soft, Non tender
CNS:- Intact
Neck stiffness:- No
Kernig sign :- No
Reflexes Right Left
Biceps. Absent. Absent
Triceps 1+ 1+
Supinator. 1+. 1+
Knee. 2+. 2+
Ankle. 1+. 1+
Plantar. Mute. Mute
Tone :- Right. Left
Upper limb. Normal. Normal
Lower limb. Normal. Normal
Power:- Right Left
Upper limb. 5/5. 5/5
Lower limb. 5/5. 5/5
- No finger nose in coordination
- No knee - heel in coordination
GAIT VIDEO:-
https://youtube.com/shorts/aOUKlG0NHu8?feature=share
LUMBAR PUNCTURE DONE ON 17/02/22
INVESTIGATIONS:-
Hemogram:-
Hb:- 13.3gm/dl
TC:- 9,200
N/L/E/M/B:- 80/15/03/02/00
MCV:- 81.1
MCHC:- 34.7
RBC count:- 4.7 millions
Platelets :- 4.3 lakhs
Aptt:- 35sec
Bleeding time :- 2min
Clotting time :- 4 min 30 sec
Prothrombin time :- 18
INR :- 1.3
RBS:- 114mg/dl
LFT:-
TB:- 0.81
DB:- 0.20
AST :- 28
ALT:- 18
AlP:- 96
TP:- 7.0
A/G Ratio:- 1.48
RFT:-
Urea :- 27
Creatinine :- 0.7
Na :- 141
K:- 4.4
Cl:- 97
CSF ANALYSIS:-
Sugar:- 74mg/dl
Protein:- 27mg/dl
Chloride:- 118mmol/L
TC:- 25 cells
DC:- 100% L
RBC - Nil
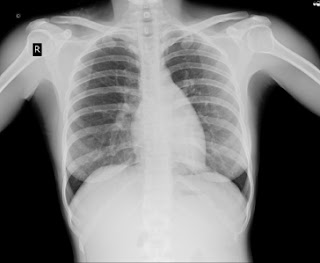
Chest X ray:-
Treatment plan:
-Inj DEXA 2cc IV STAT
-Inj CEFTRIAXONE 2gm IV/ STAT
-Inj OPTINEURON 1amp in 100ml NS IV/OD
-Inj Mannitol 20gm/ 100ml IV/ STAT
DURING CURRENT ADMISSION (27/6/2023):
Since the patient got discharged 1 year ago, she has been having intermittent fevers, 1-2 episodes a month, low grade, occasionally associated with chills and rigors. During these episodes, she would take Tab. DOLO 650mg, following which the fever would subside. The fever was not associated with nausea, vomiting.
She had intermittent episodes of headaches as well, usually during fever episodes but sometimes without fever as well, diffuse in nature, dull aching type, sometimes radiating to neck, with no aggravating factors. Patient noted that the headache was relieved after she wore her spectacles. Her headache was not associated with photophobia, phonophobia, lacrimation.
She also had tingling in both her lower limbs uptil thighs, intermittent in nature but not specifically associated with her fever. The tingling also did not have any aggravating or relieving factors as such. It was also accompanied by occasional dragging type pain in both lower limbs, non radiating in nature.
She had acute urinary retention since 1 day. She last passed urine around 1 am last night, following which she was unable to pass urine, even though she was able to feel fullness of her bladder. Retention was relieved after passing Foley's- she voided around 500ml.
She had an abortion 6 months ago, 3 months into her pregnancy. That was the only time she visited a hospital in the last year.
PAST HISTORY
She had an LSCS 3 years ago
No history of HTN, CVD, CAD, thyroid, TB, asthma, epilepsy
MARITAL AND OBSTETRIC HISTORY
The patient had a second degree consanguinous marriage at 16 years of age. 6 months into her marriage she conceived, following which she had a spontaneous abortion in the first trimester. The doctor had said that fetal heart rate was not heard.
After 2 years she conceived again after using medication for conception. This time she had a miscarriage in the second trimester due to ? situs inversus.
After 6 months she conceived again, this time to term. She gave birth to a live healthy baby who is now 3 years old.
After 2 years she conceived again, this time also she had a miscarriage in her first trimester due to absent fetal heart beat.
PERSONAL HISTORY:
Diet - mixed
Sleep - Disturbed since 1 year
Appetite - Decreased since 1 year, especially during fever episodes
Bowel and bladder - regular
No addictions
No allergies
PSYCHOSOCIAL HISTORY:
Patient is 22 years old
She studied till 10th grade, after which she got married at 15 years. She has been married since 7 years now, and has one 3 year old daughter. She works as a farmer, along with her husband who is also a farmer. She lives with her husband, daughter and mother-in-law.
Her daily routine consists of her waking up at 5.30am, preparing breakfast and eating around 9am. Her family usually eats rice or idli for breakfast. Following this, she goes for work at the fields or does household work until lunch which is at 1pm- patient eats rice for lunch. In the afternoons, she takes care of the buffaloes, and later comes back in the evening and prepares dinner which she eats around 8pm- usually rice and curry. She sleeps around 9pm.
However, she patient mentioned that she had been unable to sleep properly since several months, due to unknown reasons. She would wake up 2-3 times in the night and be unable to fall asleep again.
During her fever episodes also, she continues to work as well as take care of her daughter. Additionally, most of the household work is done by the patient even during fever episodes, as her mother-in-law has knee pain and hence has trouble walking. The patient felt that the fever episodes were a burden on her as she would have to continue working despite feeling lethargic and tired during these episodes.
She was initially worried 1 year ago getting fever episodes as she was worried that her myelitis would flare up again. However, she is no longer too anxious about this.
FAMILY HISTORY:
No significant history
GENERAL EXAMINATION:
Patient is conscious, coherent and co-operative.
She is moderately built and moderately nourished.
Pallor - Absent
Icterus - Absent
Cyanosis - Absent
Clubbing - Absent
No lymphadenopathy
Pedal edema- Absent
Vitals :
Temperature - 96.8 ° F
Blood Pressure -120/70 mmHg
Pulse Rate -78 bpm
Respiratory Rate - 13 cpm
Current gait in comparison to her gait during previous admission:
Gait from previous admission:
https://youtube.com/shorts/aOUKlG0NHu8?feature=share
Gait from current admission:
SYSTEMIC EXAMINATION:
CNS EXAMINATION:
HIGHER MENTAL FUNCTIONS-
Normal
Memory intact
CRANIAL NERVES-
Normal
Neck stiffness:- No
Kernig sign :- No
SENSORY EXAMINATION
Right Left
Spinothalamic
Crude touch + +
Pain + +
Temperature + +
Dorsal column
Fine touch Lost in bilateral soles
Vibration
Olecranon p 6s 5s
Styloid process 7s 10s
Tibia 4s 8s
Medial mallelous 6s 10s
MOTOR EXAMINATION
Reflexes Right Left
Biceps. + +
Triceps + +
Supinator. - -
Knee. ++ ++
Ankle. ++ ++
Plantar. Flexor Flexor
T11-12 Reflexes absent
Beaver's sign negative
Tone :- Right. Left
Upper limb. Normal. Normal
Lower limb. Normal. Normal
Power:- Right Left
Upper limb. 5/5. 5/5
Lower limb. 5/5. 5/5
Lower limb examination in detail, done to localise anatomy of lesion:
Power:- Right Left
HIPS
ILEOPSOAS (L1-L3) 5/5 5/5
ADDUCTOR FEMORIS (L5-S1) 4-/5 4-/5
G MAXIMUS (L5-S1) 4-/5 4-/5
G MEDIUS, MINIMUS (L2-L3) 4-/5 4-/5
THIGH
HAMSTRINGS (L4-S1) 4-/5 4-/5
QUADRICEPS (L3-L4) 4+/5 4+/5
ANKLE
TIBIALIS ANTERIOR (L4-L5) 4-/5 4-/5
TIBIALIS POSTERIOR (L4) 4-/5 4-/5
PERONEI (L5, S1) 4-/5 4-/5
GASTROCNEMIUS (S1) 4-/5 4-/5
FOOT, GREAT TOE
EXT. DIG. LONGUS (L5) 4-/5 4-/5
FL. DIG. LONGUS (S1, S2) 4+/5 4+/5
EXT. HAL. LONGUS (L5, S1) 4-/5 4-/5
EXT. DIG. BREVIS (S1) 4-/5 4-/5
- No finger nose in coordination
- No knee - heel in coordination
PER ABDOMINAL EXAMINATION:
INSPECTION
Suprapubic bulge +
Umbilicus : inverted
All quadrants of abdomen move with respiration
No visible peristalsis, pulsations, sinuses
PALPATION-
Abdomen soft
No local rise of temperature
Suprapubic bulge + non tender, relieved after Foley's catheterisation
No organomegaly
PERCUSSION:
Resonance note heard over all quadrants
AUSCULTATION:
Bowel sounds heard
CVS EXAMINATION: S1, S2 heard; no murmurs
RS EXAMINATION: BAE+, Normal Vescicular breath sounds heard
PROVISIONAL DIAGNOSIS:
LMN Type Neurogenic Bladder
?Recurrent Transverse Myelitis
?Neuromyelitis Optica Spectrum Disorder
EVALUATION:
Hemogram:
Hb: 9.3 gm%
TLC: 6700
PCV: 29.8
MCV: 71.0
MCH: 22.1
MCHC: 31.2
RBCs: 4.20 millions/cumm
PLT: 3.63 laks/cumm
ANA PROFILE- negative
ECG:
USG abdomen:












Comments
Post a Comment