This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 22 year old female, R/O Nakrekal, currently a student, came with the chief complaints of
1. Rashes all over her body since 5 days
2. Facial puffiness since 3 days
HISTORY OF PRESENTING ILLNESS
The patient was apparently asymptomatic 1 month back when she developed rashes over her legs and arms and abdomen after contact with something in her family's lemon field. For this, they visited a local doctor the next day, who prescribed her steroid ointment (halobetasol propionate) and oral medication, which she took for 10 days. The rashes subsided, however, blackish discoloration remained over the skin.
10 days back she developed fever which was high grade, intermittent in nature, associated chills and rigors and generalised body pains.
Additionally, she also developed vomiting 10 days ago (non bilious, nonprojectile), with 4-5 episodes per day.
She went to a local RMP 8 days back for the fever and vomiting, where she was diagnosed with typhoid associated with jaundice. She was treated symptomatically for the fever- given saline IV and paracetamol. She was asked to come back for a follow up to treat the typhoid once the fever subsided.
Her family had heard from her neighbourhood that jaundice can be cured by local herbal medication (livfit syrup?) and hence, went to the Ayurvedic doctor 6 days ago in the morning for the same. She took the medication the same day in the morning.
The next day morning (5 days ago), she woke up to see rashes all over her body which was itching and burning in nature. The rashes were red, of variable size, non-blanching in nature, and were noted all over her body ie over her limbs, chest, abdomen, back and groin. Palms and soles were spared.
On the same day, she went to the local Nakrekal hospital for the rashes, where they gave her soap, lotion and saline.
However, her condition was not improving. So, the next day evening (4 days ago), she went to the Suryapet hospital, where she was prescribed doxycycline, sucralfate and lotion, after which the itching deceased but the erythema and rashes remained.
The next day (3days ago) she developed edema in the perioral region along with mild dysphagia, with mild generalised edema all over her body. Additionally, she had two episodes of dizziness while walking to the bathroom, with blurring of vision. Hence, she was brought to our hospital.
No contact with any known typhoid patient
No H/O cold, cough, abd pain.
Normal daily routine:
Wakes up at 6am, attends her coaching class in a hostel followed by studying for the rest of the day. Currently preparing for civils.
Studied through her fever and vomiting episodes on the first two days, without taking rest as she was having exams.
PAST HISTORY
One month ago, she got similar rashes on her exposed areas (on the arms and legs) while walking through a lemon field. For this, she took steroids.
No history of DM, HTN, Asthma, TB, epilepsy
PERSONAL HISTORY
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bowel and bladder movements: hard stools being passed once every 2 days
No addictions
DRUG HISTORY
No known drug allergies
Steroids one month back for 10 days
She took saline and paracetamol 8 days back.
Herbal medication 6 days back.
Saline, soap, lotion 5 days back.
Doxycycline, sucralfate, lotion 4 days back
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
Patient was examined in a well lit room with informed consent.
She was conscious, coherent, co-operative; well oriented to time, person and place.
Moderately built, well nourished.
Pallor: absent
Icterus: present
Cyanosis: absent
Clubbing: absent
Lymphadenopathy: absent
Edema: present periorally
PR: 120bpm
BP: 90/70mmHg
RR: 20cpm
TEMP: Afebrile
SpO2: 99% at RA
SYSTEMIC EXAMINATION
CVS: S1, S2 heard, no murmurs
Respiratory: BAE positive, NVBS heard
P/A: Soft, nontender
CNS: No abnormalities detected
Cutaneous examination: Diffuse erythematous non-blanchable purpura of variable size noted all over body. Facial edema noted. No oral or genital mucosal involvement.
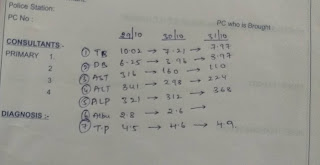
INVESTIGATIONS


























Comments
Post a Comment