This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 63 year old male, R/O Nalgonda, farmer by occupation came with the chief complaints of:
1. Shortness of breath since 10 days
2. Chest pain since 10 days
3. Fever since 2 days
Patient was apparently asymtomatic 25 years back when he started getting joint pains. They started with his right wrist first, followed by right elbow, then left wrist, then left elbow, then cervical joint, then B/L DIP, then B/L PIP, then B/L knee joint, then B/L ankle joint.
The pain increased in the morning, and decreased after some activity, around half an hour. After consulting a local RMP, he was put on NSAIDs and steroids, which he started taking.
10 years ago, he fell from a bike but sustained no injuries.
2 years ago, he had an episode of hematemesis, for which he received 2 blood transfusions.
1 year ago, he developed abdominal distension and pedal edema uptil the knee, for which he visited the hospital. It was relieved on medication.
7 months ago, he had trauma to his left leg forming an ulcer with active discharge. Culture was done, culture showed Pseudomonas. Dressing was done.
1 month ago, while walking, his legs got stuck in a rope and he fell. He went to the hospital and got an X ray done, however nothing was found. He continued to have back pain after this, dragging type, which starts in his lower back and radiates frontwards towards his chest.
Since 10 days, he has had shortness of breath, initially grade II NYHA, and progressing to grade III over the next two days. Orthopnoea and PND is present. No associated chest pain.
Along with SOB, he also developed cough since 10 days, with sputum. The sputum was moderate in amounts, white in colour, non blood tinged, non foul smelling.
He had H/O fever 2 days back, low grade, subsided on taking medication.
DAILY ROUTINE:
The patient owns a toddy farm and a normal farm, and divides his time between these two. He wakes up early in the morning and goes to his farm, then in the afternoon takes care of the toddy plants. Again in the evening, he goes to his farm again. His routine did not change until 10 days ago, when he developed shortness of breath.
PAST HISTORY
No H/O DM, HTN, asthma, TB
PERSONAL HISTORY
Diet: Mixed
Appetite: Normal
Sleep: Adequate
Bowel and bladder: Regular
No allergies
Has been smoking 1 pack beedi per day since 40 years
GENERAL EXAMINATION
Patient is conscious, coherent and cooperative and examined in a well lit room.
He is an obese individual with flexion at the PIP joints of his both right and left hand and toes.
Healed ulcer present on his left leg.
No signs of pallor, icterus, cyanosis, clubbing, edema, lymphadenopathy.
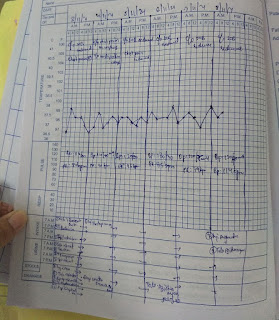
PR - 89 bpm
BP - 130/80mmhg
RR - 25cpm
Spo2 - maintaining at 89 % on Room air
Temp: Afebrile, 98 degrees
SYSTEMIC EXAMINATION
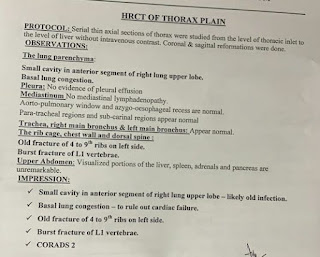
RS: BAE, wheeze present. B/L inspiratory crepts heard in all lung fields
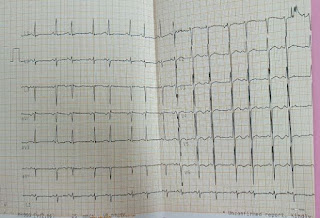
CVS: Muffled S1,S2; No raised JVP; no murmurs heard
P/A: Soft, non tender
CNS: No abnormality detected
DIAGNOSIS
HFrEF (30%) with acute COPD exacerbation, iatrogenic Cushing's Syndrome, Rheumatoid Arthritis








Comments
Post a Comment