This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 45 year old female, R/O Doomipaamulu, came with the chief complaints of
1. Slurring of speech since 1 day
2. Double vision since 1 day
3. Swelling and numbness of tongue since 1day
The patient was apparently asymptomatic 10 years ago when she had 2 episodes wherein she would not respond to anyone around her, which lasted about 5 minutes each. On going to the hospital, she was diagnosed with HTN for which she has been taking amlodipine.
She was also diagnosed with DM 6 years ago. Following a hysterectomy, her sutures were not healing and on going to the hospital, she was found to be diabetic. She has been on medication ever since ( Glimiperide).
15 days ago, she fell on a bucket while she was mopping and sustained an injury to her left hypochondriac region, following which she had pain in the same region. The following day, she went to a local doctor and received two painkiller injections. However, the pain did not subside, hence she went to another doctor 13 days later.
The second doctor, on performing a scan, said that the bone was not involved, and that it was most likely a muscle pain, hence gave her another painkiller injection. After taking the injection, the patient went home.
However, within thirty minutes, after she had reached home, she developed slurring of speech, which was sudden in onset. She also felt that her tongue was swollen.
The attender noted that she already seemed to have an unsteady gait on the way home itself.
Additionally, the patient felt dizzy, which was sudden in onset.
She also noted double vision, sudden onset, binocular diplopia.
No h/o seizures, headache, vomiting, dysphagia, palpitations.
DAILY ROUTINE:
Wakes up at 6am, does her household work. Some days, she goes out for work as she is the president of her local MPTC (Mandal Parishad Territorial Constituency). On other days, she spends the day at home playing with her grandchildren.
PAST HISTORY
No similar complaints in the past.
H/o DM (6yrs), HTN (10yrs).
No H/o TB, Asthma, epilepsy, CAD.
PERSONAL HISTORY
Diet: Mixed
Appetite:Normal
Sleep:Adequate
Bowel and bladder:Regular
No known drug allergies, addictions
GENERAL EXAMINATION
Patient is conscious, coherant, cooperative, well oriented to time, place and person.
Moderately built and nourished.
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema.
VITALS:
Temperature: Afebrile
PR: 77 bpm
BP: 130/80 mmHg
RR: 19 cpm
SpO2: 99%
GRBS: 229mg/dl
SYSTEMIC EXAMINATION:
RS: BAE, NVBS
CVS: S1, S2 heard, no murmurs
P/A: Soft, non tender
CNS:
1. Speech: slurred
2. Cranial nerve examination: normal
3. Sensory: normal in all dermatomes
4. Motor:
a. Tone normal
b. Power 5/5 in b/l lower limbs; 5/5 in b/l upper limbs
5. Reflexes: normal
6. Cerebellum:
a. Not able to perform rhomberg's (as she sways even with eyes open)
b. Finger nose test normal
c. No dysdiodokinesia
7. Nystagmus present: gaze evoked, horizontal more on right gaze with fast component towards the right, and seen with upward gaze- vertical upbeat and downbeat +
8.Gait: slow paced, swaying on both sides.
9. Stride:regular with path deviation
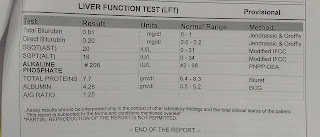
INVESTIGATIONS:
PROVISIONAL DIAGNOSIS:
Lesion at the level of pons and cerebellum.
TREATMENT:
1. Tab. ECOSPRIN 150mg PO/OD
2. Tab. CLOPIDOGREL 150mg PO/OD
3. Inj. NPH S/C BD 20U
4. Inj. HAI 10U-10U-8U
5. Tab. BPLEX FORTE OD





Comments
Post a Comment