This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 65 year old male, labourer by occupation, r/o gudigade came with the chief complaint of:
1. Shortness of breath since 3 days
Tha patient was apparently asymptomatic 3 years back when he developed pedal edema uptil the knee, for which he went to the hospital. On performing investigations, he was diagnosed to be hypertensive, and he was told that his kidneys were failing, and dialysis was suggested.
Following this, they went for a second opinion to Khammam, where the same diagnosis was made. Hence, they came to our hospital to start dialysis.
They had been getting hemodialysis done since 3 years- two times a week. No previous complications had been noted.
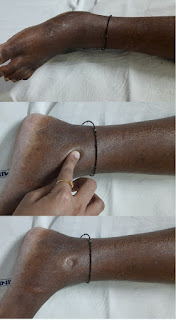
Since 4 months, he had left upper limb swelling, which gradually progressive. Additionally, he also developed mild swelling in the chest 4 months ago, which was also gradually progressive.
Since 2 months, he has been having back pain from base of the neck till mid back, which was intermittent in nature. It subsided on taking medication (Tab ultracet)
3 days ago, the patient started having SOB right after his dialysis, while he was still in the hospital. The SOB was grade IV NYHA, with no specific aggravating or relieving factors. Since he was having SOB, the patient decided to stay overnight in the hospital and go back home the next day. However, his condition did not improve and he was hence admitted and put on ventilatory support. The patient additionally complained of chest pain, which was persistent and of dull aching type, with no radiation.
There was no h/o decreased urine output, orthopnea, PND or palpitations.
The patient stopped working 3 years ago following his CKD diagnosis and decided to stay at home. His wife would go to work instead.
PAST HISTORY
No similar complaints in the past
No h/o DM, asthma, thyroid problems, seizures
PERSONAL HISTORY:-
Diet: Vegetarian since 3 years, after his CKD diagnosis
Appetite: Normal
Sleep: Adequate
Bowel & bladder: Regular
No allergies
Used to drink toddy everyday until 3 years ago
FAMILY HISTORY:
Insignificant
GENERAL EXAMINATION:
Pt is conscious, coherent, cooperative
Well oriented to time, person, place
Moderately built, well nourished
Pallor +
Pedal edema +
No Icterus/cyanosis/clubbing/Generalized lymphadenopathy
VITALS:
Temp: Afebrile
PR: 83bpm
RR: 18cpm
BP: 110/60 mmHg
General examination on admission:
General examination after 1 week:
Fever chart:
SYSTEMIC EXAMINATION:
CVS: S1 S2 heard, No murmurs
RS: BAE+, NVBS, no adventitious breath sounds
P/A: soft, non tender
CNS: NAD, normal higher functions
ECG on admission:
STEMI, LAD blockage noted. (V1,2,3,4)
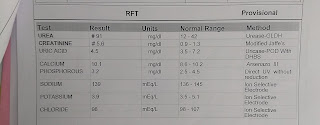
INVESTIGATIONS on admission
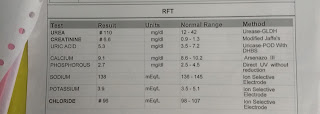
AFTER 2DAYS:
Pleural tap was done.
PLEURAL TAP:
MEDICATION THAT HE IS CURRENTLY ON:
1. NICARDIPINE, CLONIDINE- HTN
2. ACILET (SODIUM BICARB), CALCITRIOL, FUROSEMIDE: CKD
3. ULTRAKING (PARACETAMOL AND TRAMADOL): ANALGESIA
PROVISIONAL DIAGNOSIS:
K/C/O CKD on MHD, HTN
Lateral wall MI
?Spondylodiscitis
?Left Upper Limb lymphedema (secondary to AV fistula surgery)
TREATMENT PLAN:
-T Lasix 40mg/PO/BD
-T Nicardia 10mg/PO/TID
-Inj EPO 4000IU once weekly
-Inj Iron sucrose 100mg in 100ml once weekly
-T MVT PO/OD
-T NODOSIS 500mg PO/OD
-T OrofexXT OD
- T BioD3 OD
-T Dolo 650 SOS
-T Ultracet BD
























Comments
Post a Comment