This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
18 year old female came with chief complaints of:
1. Fever since 3months
2. Joint pain since 3 months
3. Headache since 3 months
4. Vomitting episodes since 10 days
Patient was apparently asymptomatic 3 months ago when she developed fever, which was persistent in nature, low grade. However, one-two times a week, she would have exacerbations if the fever, wherein the fever would suddenly become high grade and associated with chills and rigors. It would decrease on taking medication e, high grade. Once the fever subsided, the patient started having pain in the small joints, for which she took medication. Once she stopped the medication, the pain would come back. Following small joints (PIP, DIP), the pain progressed to include even elbow and shoulder joints, which was associated with exacerbation of fever episodes.
She also had h/o headache since 2 months, intermittent in nature, usually during her fever episodes.
H/o decreased appetite since 2months ,along with h/o pain abdomen 15 days ago, which subsided in 2-3 days. Along with the abdominal pain, she also had a few episodes of vomitting, which was non bilious, non projectile.
Following these symptoms, she came to our hospital where she was evaluated and a diagnosis of SLE was made. She was given appropriate treatment in the form of ultracet, HCQ and was discharched on 7th February. However, following the discharge, she started having episodes of vomitting again (nonbilious, nonprojectile) with associated nausea, most likely due to HCQ intolerance. She stopped taking HCQ on 11th and shifted to T. onmacortil for 2-3days, however, as the vomitting did not subside, she stopped taking that as well. 3 days later, she presented to our hospital.
PAST HISTORY
No similar complaints in the past
No h/o DM, HTN, asthma, thyroid problems
PERSONAL HISTORY:-
Diet: Mixed
Appetite: Decreased since 2months
Sleep: Adequate
Bowel & bladder: Regular
No addictions/allergies
FAMILY HISTORY:
Insignificant
GENERAL EXAMINATION:
Pt is conscious, coherent, cooperative
Well oriented to time, person, place
Moderately built, well nourishes
Pallor +
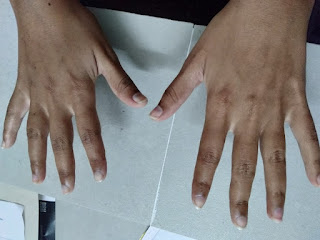
No Icterus/cyanosis/clubbing/Generalized lymphadenopathy/pedal edema
VITALS:
Temp: Afebrile
PR: 83bpm
RR: 18/min
BP: 110/60 mmHg
Spo2- 98%at RA
SYSTEMIC EXAMINATION:
CVS: S1 S2 heard, No murmurs
RS: BAE+, NVBS, no adventitious breath sounds
P/A: soft, non tender
CNS: NAD, normal higher functions
Skin: Erythematous rash on malar prominence and nasal bridge
Joints: Mild swelling over L elbow
INVESTIGATIONS (done before 7/2/2022):
ANA, dsDNA positive
Low C3, C4
Direct COOMBs positive
LDH mild increase
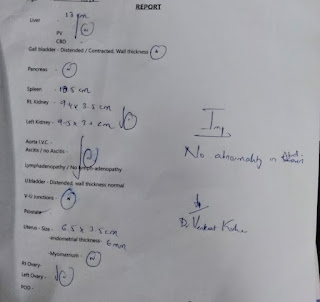
INVESTIGATIONS (Done after readmission on 14/2/2022):














Comments
Post a Comment