This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 44 year old male, farmer by occupation cane with the chief complaints of
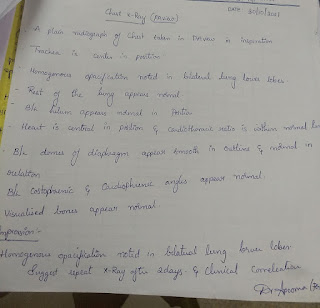
1. Shortness of breath since 10 days
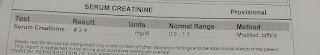
Patient was apparently asymptomatic 10 years back when he was diagnosed with CKD and has been on regular medication ever since.
Additionally, he was diagnosed with DM 5 years back when he went to the doctor with C/O stabbing-type chest pain, for which he has been taking glimepiride.
He was also diagnosed with HTN 1 year back after he had an episode of dizziness with blurring of vision and tachycardia. On visiting the local doctor, he was told that his BP was 160/90mmHg and he was prescribed telmesartan.
He also complained of leg pain since 1month, which was intermittent in nature, throbbing type pain, non radiating, decreased on rest and increased on exercise.
2 weeks ago, he developed fever which was high grade, associated with chills and rigors, and 2 episodes of vomitting (non bilious, non projectile). On visiting the hospital, he was diagnosed with typhoid and treated accordingly with antibiotics. Typhoid was not associated with jaundice, constipation.
10 days back, he developed SOB (grade 2 NYHA) which has no noted aggravating or relieving factors. Not ass with orthopnoea, PND, or cough. No chest pain was noted.
There was also bilateral pedal edema (pitting) since 1 week
Facial puffiness since 1 week
Decreased urine output since 1 week
Epigastric pain since 1 week, with c/o abdominal distention
DAILY ROUTINE
He is a farmer (cotton), and also owns a Kirana shop on the side. Additionally, he works as a watchman between the months of October and March.
Since the pandemic, however, he stopped his duties as a watchman owing to lack of time management, and his hypertension diagnosis.
He usually wakes up at 6am, tends to his farm, had lunch and then goes to his shop for the rest of the evening. Since 2 weeks, however, he has not been going to his shop.
PAST HISTORY
CKD- 10yrs
DM- 5yrs
HTN- 1yr
PERSONAL HISTORY
Diet: Mixed
Appetite: Normal
Sleep: Disturbed
B&B: Regular
Used to smoke (15-20 per day) and drink (quarter per day) but he stopped 10 years ago.
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
C/C/C, well oriented to time, place, person
Overweight, moderately built
Clubbing present
Pallor, icterus, cyanosis, lymphadenopathy, edema absent
VITALS
Temp: Afebrile
PR: 89bpm
RR: 2cpm
BP: 130/80mmHg
SpO2: 98% @ RA
SYSTEMIC EXAMINATION
CVS: S1, S2 heard. JVP raised. Apex beat not localised properly. Epigastric pulsations felt.
RS: NVBS + , BAE +
P/A: Soft, nontender
CNS: No abnormalities foun
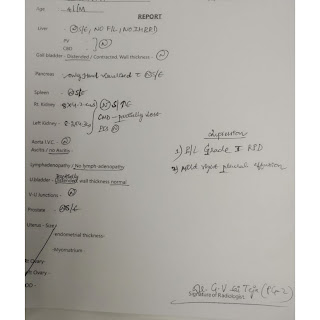
PROVISIONAL DIAGNOSIS:
Heart failure with preserved ejection fraction (45%) with CKD since 10 years, DM since 5 years, HTN since 1 year
TREATMENT
1. Salt restriction (2.5g/day)
2. Fluid restriction (<1l/day)
3. Inj. Lasix 40mg/IV/BD
4. Inj Pantop 40mg/IV/OD
5. Tab. shelcal 500mg/OD
6. Tab.Nododsis 550mg/PO/OD
7. Tab. PCM 500mg/PO/SOS
8. Inj. Piptaz 2.25g/IV/BD
9. Inj Neomol 100ml/IV/SOS









Comments
Post a Comment