This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 70 year old male, resident of Nalgonda, coal miner by occupation cane with the chief complaints of:
1. Fever since 15 days
2. Shortness of breath since 10 days
3. Cough since 10 days
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 15 days back when he developed a fever, sudden in onset, intermittent with a rise in temperature at night, associated with chills and rigors. No aggravating factors were noted, relieved on taking Tab. Paracetamol.
He noted a history of Shortness of Breath since 10 days, insidious in onset, Grade III (NYHA classification) with was aggravated on working and relieved on rest. There was no associated diurnal or positional variation, or paroxysmal nocturnal dyspnoea.
He also had a history of cough since 10 days, associated with copious amounts of whitish sputum, non-foulsmelling and non-bloodtinged.
He had no history of chest pain.
PAST HISTORY
One episode of dull-aching chest pain with palpitations 10 years back, for which angiogram was performed. He has been taking statins since then.
History of HTN since 5 years, for which he takes amlogen (CCB) regularly.
History of Type2 DM since 2 years, for which he takes glimepiride.
History of asthma- since 2 years, for which he has been using an inhaler.
No history of TB, epilepsy, thyroid dysfunction.
PERSONAL HISTORY
Diet: Mixed
Appetite: normal
Sleep: decreased
Bowel and bladder movements: regular
Addictions: Smoking since 50 years, stopped since 2 years. Takes alcohol everyday since 40 years, between 50-100ml.
No known food or drug allergies
FAMILY HISTORY
Insignificant
GENERAL EXAMINATION
Patient conscious, coherent, cooperative
Well oriented to time, person, place
Moderately built, well nourished
No pallor, icterus, cyanosis, clubbing, lymphadenopathy
B/L pedal edema- uptil knee
Vitals:
PR- 112bpm
BP- 140/80mmHg
RR- 20cpm
SpO2- 98% at room atm
SYSTEMIC EXAMINATION
CVS: S1, S2 heard
PA: Soft, nontender
CNS: no abnormalities found
RS: BAE+, with expiratory wheeze present in supra, inter, Infrascapular areas bilaterally
PROVISIONAL DIAGNOSIS
Viral pyrexia with chronic bronchial asthma with lung pathology under evaluation
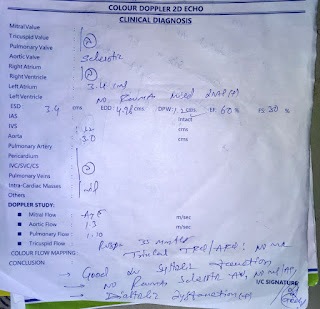
Diagnosis: Viral Pyrexia with Pneumoconiosis (occupational lung disease)
TREATMENT
1. O2 supplementation
2. Nebulisation with duolin 6hrly, Budecort 8hrly
3. Inj Pan 40mg IV OD
4. Syrup Ascoryl TID
5. Tab Prednisolone 5mg OD
6. Inj Monocef 1gm IV BD
7. Tab Azithromycin 500mg OD
8. Tab dolo 650mg BD
9. I/O monitoring




Comments
Post a Comment