A 40 Year Old Male with Complaints of Irrelevant Talking
This is an online E-log entry blog to discuss and understand the clinical data analysis of a patient, to develop competency in comprehending clinical problems, and providing evidence- based inputs in order to come up with a diagnosis and effective treatment plan to the best of my ability.
A 40 year old male presented to the hospital from Yadagirigutta with the chief complaints of irrelevant talking and decreased food intake since 9 days.
HISTORY OF PRESENTING ILLNESS:
The patient was apparently asymptomatic 9 days ago, when he started talking, as well as laughing to himself, which was sudden in onset. He was conscious, but oriented to time, person and place only from time to time. He was unable to lift himself off the bed and move around, and had to be assisted. It was associated with a decrease in food intake since 9 days. Following this, he was taken to a local RMP, given IV fluids, and referred to a higher care hospital. He had also stopped drinking the same day, citing general body pains the day before.
His last alcohol intake was on Monday, when he had drank around 1 bottle.
He also had short term memory loss since 9 days, where he could not recognize family members from time to time.
Previously, he had 2-3 episodes of seizures, one being 1 year ago and the most recent being 4 months ago. The most recent time, (4 months ago), he had developed seizures (most probably GTCS) following cessation of alcohol for 24 hours, which was associated with restlessness, sweating, and tremors. Following this episode, he started drinking again.
He was admitted to a tertiary care hospital on 15th May.
PAST HISTORY:
-History of 2-3 episodes of seizures in the last year, most likely due to alcohol consumption
-K/C/O Type 2 Diabetes since 2 years, for which he has been irregularly taking tablets (once in 2 or 3 days)
-No similar complaints in the past
No history of hypertension, CAD, TB or asthma
PERSONAL HISTORY:
Diet: Mixed
Appetite: Decreased
Sleep: Disturbed
Bowel and bladder: Regular
Addicted to alcohol, drinks about 3-4 quarters per day- since 12 years
Addicted to cigarettes, smokes around 10 per day
DRUG HISTORY
On oral hypoglycemic for DM2 since two years, tablets being taken irregularly
No known drug allergies
FAMILY HISTORY:
No similar complaints in the family
No H/O psychiatric illness in the family
GENERAL EXAMINATION: (at the time of admission)
The patient was examined in a well lit room, with informed consent.
Conscious and co-operative, but not coherent.
Not oriented to time, person and place.
Speech is normal, but talks about irrelevant things.
Moderately built and well nourished.
Pallor: Absent
Icterus: Absent
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: Absent
Edema: Absent
Pupils: Normal in size, reactive to light
Vitals:
16/05/21 17/05/21 18/05/21 19/05/21
HR: 110bpm HR: 101bpm HR: 110bpm HR:84bpm
BP: 100/60mmHg BP:100/70mmHg BP: 110/70mmHg BP: 150/90mmHg
Temp: Febrile on touch Temp: One spike at 7am Temp: Afebrile Temp: Afebrile
SYSTEMIC EXAMINATION: (at time of admission)
CVS: S1, S2 heard
Respiratory: Bilateral Air Entry positive
Per Abdomen: Soft and non-tender, bowel sounds heard
INVESTIGATIONS:
1. CXR-PA view
2. ECG report
3. CBP
-Hb: 11.1g% (decreased) -MCV: 90.2fl
-WBC: 18,300 cells/cumm -MCH: 32.6pg (increased)
-Platelet count: 1.51 lakh/cumm -MCHC: 34.6% (increased)-PCV: 32.1% (decreased)
4. Urinary Chloride, Sodium, Potassium
-Chloride: 375 mmol/L
-Potassium: 16.4 mmol/L
-Sodium: 244 mmol/L
-Ketone bodies absent in urine
5. CUE
-Normal
6. Serum electrolytes
7. LFT
8. RFT
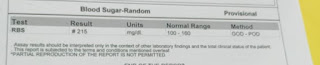
9.RBS
10. ABG
10. 2D ECHO
-Mild LV hypertrophy
11. USG abdomen
-Bilateral Grade1 RPD
-Echogenic intramural foci noted in gallbladder
REFERRAL TO PSYCHIATRY:
-Patient told wife that he saw his brother (who expired recently) and was talking to him.
-H/O multiple involuntary movements associated with rolling of eyes, frothing, tongue bite, loss of consciousness.
-No H/O suspiciousness, pervasive mood, suicidal ideation, grandiosity, repetitive thoughts.
Examination:
-Patient is anxious, lying on the bed. Tremors present.
-Conscious, coherent, co-operative. Well oriented to time, place, person.
-Established rapport, answers questions but talks irrelevant things.
-Thought and perceptions could not be established.


















Comments
Post a Comment